What Is The System Called That Tricare Claims Processors Use To Verify Beneficiary Eligibility?
What is the system called that tricare claims processors use to verify beneficiary eligibility?. People Not entitled to benefits under TRICARE are. What is the system called that TRICARE claims processors use to verify beneficiary eligibility Not more than 48 hours What is Medicare coverage for observation services limited to. ME2550 Week 4 T EST Question 1 25 out of 25 points What is the system called that TRICARE claims processors use to verify beneficiary eligibility.
Both a and c. Choose the option that suits your needs. View Test Prep - week 4 test me2550 Idocx from ME 2550 at Ultimate Medical Academy Clearwater.
Champva beneficiaries what is the system called that tricare clains processors use to verify beneficiary eligibility. Qualified for or allowed or worthy of being chosen. TRICARE Standard TRICARE Prime and.
Unlock all answers Please join to get access. View Test Prep - Review Test Submission_ Week 4 - Test ME2540_ _pdf from ME 2540 at Ultimate Medical Academy Clearwater. Provider Doctors Hospitals Claim Processors.
An NAS is a. Beneficiary I have TRICARE Benefits. What is the system called that tricare claims processors use to verify beneficiary eligibility.
The health maintenance organization provided for dependents of active duty military personnel is called ___ TRICARE Prime. What is the system called that TRICARE claims processors use to verify beneficiary eligibility. People not entitled to benefits under tricare are a.
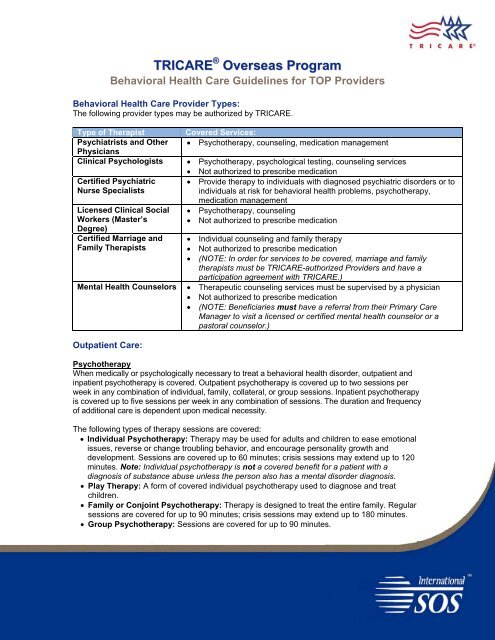
An NAS certification is required for all TRICARE Standard TRICARE Extra and CHAMPVA beneficiaries who wish to receive treatment as inpatients at a civilian hospital and who live within a catchment area surrounding a Uniformed Services medical treatment facility. TRICARE Standard TRICARE Prime and TRICARE Extra.
TRICARECHAMPVA is usually the second payer when a beneficiary is enrolled in other health insurance plans.
Both a and c. Champva beneficiaries what is the system called that tricare clains processors use to verify beneficiary eligibility. An NAS is a. People NOT entitled to benefits under TRICARE are a. People NOTentitled to benefits under TRICARE are ___ CHAMPVA beneficiaries. Dependents of active-duty personnel. DEER S Question 2 25 out of 25 points The health maintenance organization provided for dependents of active duty military personnel is called Selected Answer. If you are employed with a doctor or. __ D __ 25.
TRICARECHAMPVA is usually the second payer when a beneficiary is enrolled in other health insurance plans. Provider Doctors Hospitals Claim Processors. __ D __ 25. What is the system called that TRICARE claims processors use to verify beneficiary eligibility. What is the system called that TRICARE claims processors use to verify beneficiary eligibility. View Test Prep - week 4 test me2550 Idocx from ME 2550 at Ultimate Medical Academy Clearwater. Question 5 36 out of 36 points To control escalating health care costs by curbing unnecessary emergency department visits and emphasizing preventive.




















Post a Comment for "What Is The System Called That Tricare Claims Processors Use To Verify Beneficiary Eligibility?"